If you have diabetes, you’re at higher risk of developing foot problems, including open sores, infections, and other complications. Poor blood circulation, nerve damage (neuropathy), and altered pressure on your feet can make even small injuries serious. That’s why early detection and management are crucial. Visiting a podiatrist can help you prevent, identify, and treat early diabetic foot issues before they escalate. Through routine foot checks, preventive care, and advanced diagnostics, podiatry provides targeted solutions to maintain healthy feet and minimise the risk of severe complications.
At MyFootDr Singapore, our experienced podiatrists deliver evidence-based care and personalised treatment plans to help you manage and prevent diabetic foot problems. Read on to discover everything you need to know to keep your feet healthy.
What Are Diabetic Foot Problems?
Diabetic foot problems are complications that can arise when high blood sugar levels persist over time. People with diabetes are at higher risk of developing foot issues, especially if they have nerve damage (neuropathy) or poor circulation. Neuropathy can reduce sensation in the feet, making it harder to notice cuts, blisters, or injuries. These unnoticed wounds can easily become infected and cause more complications.
Diabetes can also slow healing because of reduced blood flow and a weakened immune system, which may allow infections to worsen or spread. If left untreated, severe complications like gangrene or even amputation can occur. Being aware of the risks and taking proactive care of your feet, along with proper diabetes management, can significantly reduce the chance of serious foot problems. Simple preventive measures, regular foot checks, and early treatment of injuries are essential to keeping your feet healthy.
How Does Diabetes Affect Your Feet?
Nerve damage and poor circulation are the two main reasons why people with diabetes need regular foot checks and early podiatry care to avoid serious complications. Diabetes mainly causes two conditions that can significantly affect foot health:
- Diabetic Neuropathy
Long-term high blood sugar can damage the nerves in your feet and legs, reducing your ability to feel pain, heat, or cold. This lack of sensation means you may not notice cuts, blisters, or pressure points caused by tight shoes. Over time, unnoticed wounds can become infected. Nerve damage can also affect the muscles in your feet, leading to misalignment and uneven pressure, which increases the risk of ulcers. - Peripheral Vascular Disease
Diabetes also reduces blood flow to the feet by narrowing blood vessels. Poor circulation makes it harder for wounds to heal, so even small injuries can take much longer to heal. If infections don’t heal properly, they can spread and cause ulcers or even gangrene, which is the death of tissue due to a lack of blood supply.
Spotting Early Signs of Diabetic Foot Problems
Catching foot problems early is one of the best ways to prevent serious complications from diabetes. Many issues start small but can quickly worsen if ignored. That’s why it’s important to check your feet daily and look out for these warning signs:
- Changes in Skin or Nails: Redness, swelling, blisters, cuts, or ingrown toenails can be the first sign of infection. Dry or cracked skin can also allow germs to enter.
- Slow Healing Wounds: Open sores, ulcers, or injuries that don’t heal or continue draining fluid/pus need urgent medical care.
- Swelling and Pain: Persistent swelling in the foot or ankle, or pain in the feet and legs, could point to poor circulation or infection.
- Changes in Foot Shape or Colour: Sudden changes in how your foot looks, or darkened skin, may indicate more serious complications.
- Unusual Odour: A persistent foul smell or foot odour that doesn’t go away may also indicate a foot infection.
Common Foot Problems That Are More Risky with Diabetes
Anyone can experience foot problems, but for people with diabetes, even minor issues can become serious. Poor circulation and nerve damage mean cuts, sores, or pressure spots may not heal properly, increasing the risk of infection and even amputation. Here are the most common foot conditions linked to diabetes and why you should never ignore them:
Fungal Infections (Athlete’s Foot & Nail Fungus)
Diabetes makes fungal infections riskier. Athlete’s Foot causes itching and cracks between the toes, while fungal nail infections make nails thick, brittle, and hard to treat. Both may require antifungal creams, oral medicines, or in severe nail cases, removal.
Skin Buildups (Calluses & Corns)
Excess pressure on the feet leads to thickened skin. Calluses can turn into ulcers if ignored, while corns are painful cone-shaped buildups caused by friction. Safe podiatry care, proper footwear, and cushioned pads can help prevent complications.
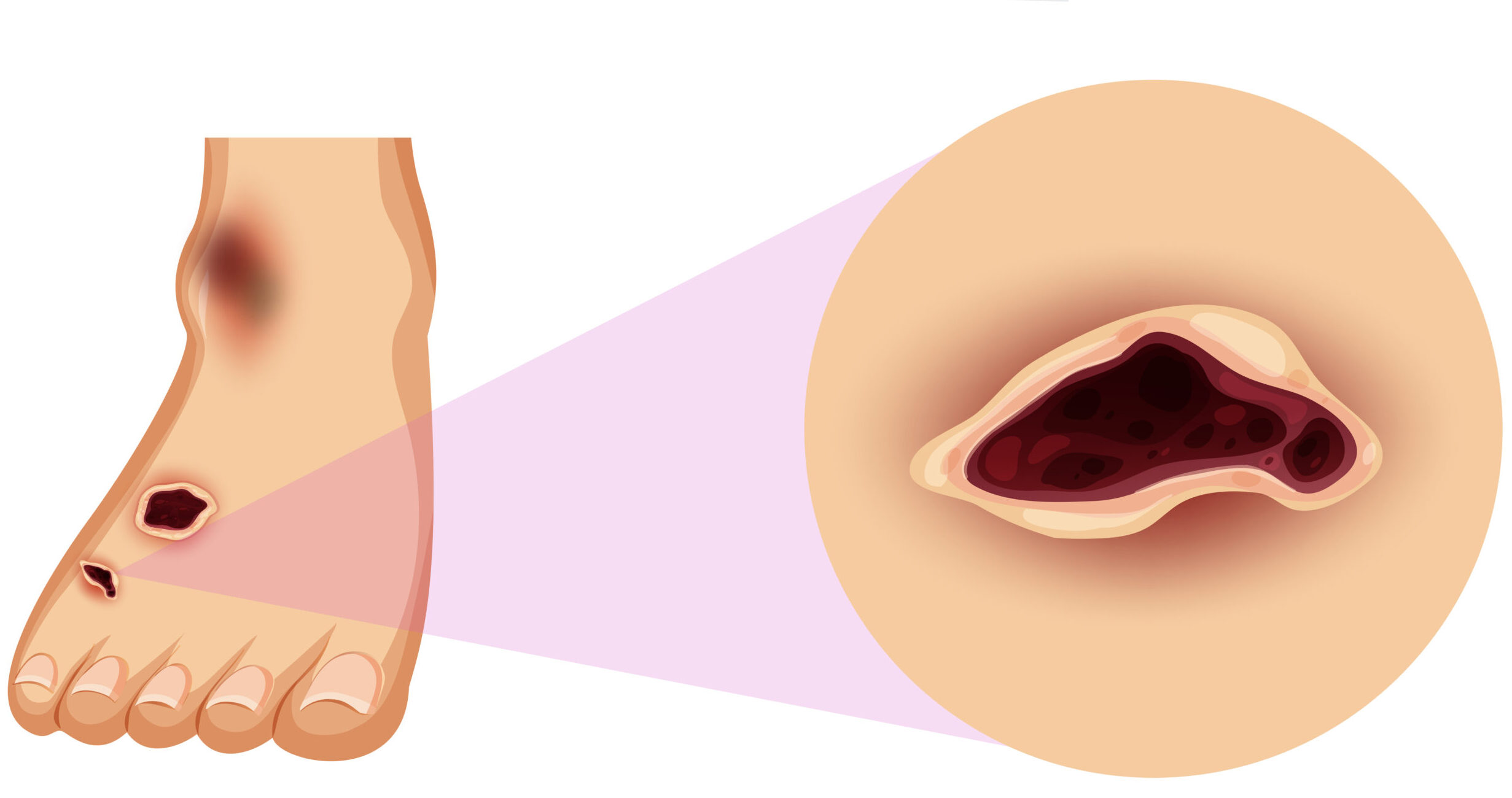
Blisters & Foot Ulcers
Blisters from friction or diabetic blisters may seem minor but can get infected easily. Ulcers, on the other hand, are deep wounds that heal poorly and often lead to serious infections. Both require prompt medical attention, with ulcers needing urgent care.
Toe Problems (Hammertoes & Ingrown Nails)
Hammertoes curl downward due to weakened muscles, causing pain and sores, while ingrown toenails lead to redness, swelling, and infection. Special shoes, splints, or minor surgery may be needed depending on severity.
Plantar Warts
Viral infections that cause hard, painful growths on the heel or ball of the foot, often mistaken for calluses. They may show black dots in the centre and require freezing, medication, or minor surgery for removal.
Swelling (Oedema)
Poor circulation, kidney issues, or medications can cause feet and ankles to swell, increasing the risk of skin breakdown. Elevating feet, wearing compression socks, staying active, and lowering salt intake can help manage it.
Complications of Untreated Diabetic Foot Problems
If diabetic foot problems are ignored or left untreated, they can progress into severe and sometimes life-threatening complications. Even something as small as a blister or cut can escalate quickly due to poor blood circulation, nerve damage, and slower healing. Here are some of the most common complications:
- Skin and Bone Infections
Small wounds can easily become infected because diabetes weakens blood vessels and the immune system. While infections can often be treated with antibiotics, severe cases may require hospital care. - Abscess
If an infection spreads deeper into the tissue or bone, it can form an abscess, a painful pocket of pus. Treatment usually involves draining the abscess, and in some cases, removing affected bone or tissue. Less invasive options like oxygen therapy may also be used.
- Gangrene (Tissue Death)
When blood flow to the foot is severely reduced, tissue can die, causing the skin to turn black. Gangrene is a medical emergency that often requires surgery or oxygen therapy to remove the affected area.
- Foot Deformities
Nerve damage can weaken foot muscles, leading to structural problems like hammertoes, claw feet, prominent bone ends, or a high arch that doesn’t flatten with weight-bearing. These deformities increase the risk of pressure points, wounds, and ulcers.
- Charcot Foot
Diabetes can weaken bones in the foot until they fracture. Because nerve damage reduces sensation, people may continue walking on broken bones without realising it. Over time, the arch of the foot can collapse into a rocker-bottom shape, making walking difficult. - Amputation
In the most severe cases, when infections cannot be controlled, abscesses develop, or blood flow is severely compromised, leading to gangrene, amputation of part of the foot or leg may be necessary. This is a last-resort treatment to prevent life-threatening complications.
Treatments for Diabetic Foot Problems
The right treatment for diabetic foot problems depends on how early they are detected and how severe the condition is. In most cases, the earlier you seek care, the easier it is to prevent complications. Treatment may include a combination of self-care, medical management, and sometimes surgery. One of the most important things to remember is not to treat these conditions yourself. Always seek medical help from a podiatrist who specialises in foot care.
Professional Wound Care
For diabetes-related ulcers, your podiatrist will carefully clean the wound, drain any fluid or pus, and remove dead or infected tissue through a process called debridement. They may also apply special dressings and ointments designed to absorb excess fluid, protect the wound from further damage, and promote faster healing.
Medications
Antibiotics, either oral or intravenous, are commonly prescribed to treat infections in diabetic foot problems. Pain management is also an important part of treatment, while over-the-counter medications such as acetaminophen or ibuprofen can help with general discomfort, prescription medicines like pregabalin, gabapentin, or certain antidepressants may be recommended for nerve pain. Additionally, topical options such as lidocaine patches or capsaicin cream can provide targeted relief for neuropathy symptoms.
Advanced Therapies and Surgery
In some cases, diabetic foot problems may require hospital care, especially if infections spread or do not heal with standard treatment. Surgical procedures might be needed to drain abscesses, correct foot deformities, or remove severely damaged tissue. In extreme situations where infection or gangrene cannot be controlled, amputation may be the only option, though with early diagnosis and proper treatment, this risk can be significantly reduced.
Manage Early Diabetic Foot Problems
Catching diabetic foot issues early can make a huge difference in preventing serious complications. The key is consistent self-care at home combined with timely medical support. Here are some practical steps for managing early foot problems:
- Proper Wound Care
Even minor injuries should be cleaned gently and covered with a sterile bandage. Don’t use harsh antiseptics or attempt to cut away damaged skin yourself. If you notice delayed healing, increasing redness, or pus, seek medical care promptly. - Wear Supportive Footwear
Choose shoes that fit properly, with soft insoles and enough room for your toes. Avoid walking barefoot, even indoors, to reduce the risk of accidental cuts or blisters. - Maintain Good Blood Sugar Levels
Keeping your blood glucose under control is one of the most effective ways to protect your feet. Stable blood sugar supports nerve health and improves circulation, reducing the risk of both neuropathy and slow-healing wounds. - Go for a Diabetic Foot Screening at the Podiatrist
Regular check-ups with a podiatrist can help identify early signs of problems you may not notice yourself, such as loss of sensation, changes in foot structure, or poor circulation. These screenings allow for preventive care before complications develop. - Seek Early Medical Advice
If you spot any changes in your feet that don’t improve within a day or two, schedule an appointment with a podiatrist. Early treatment helps prevent ulcers, infections, and more severe complications.
Choose MyFootDr Singapore for All Your Foot Treatment and Care
Living with diabetes can feel overwhelming, especially when foot problems begin to affect your daily comfort and mobility. At MyFootDr Singapore, our podiatrists understand the unique challenges of diabetic foot care and are committed to helping you protect your feet at every stage. Our team combines medical expertise with advanced technology to detect problems early, promote faster healing, and prevent complications such as ulcers or amputation.
Whether you’re managing mild symptoms like dry skin or more complex issues like neuropathy and ulcers, our podiatrists will create a personalised treatment plan to keep your feet healthy and strong. Don’t wait until your diabetic foot problems get worse. Schedule a diabetic foot screening with MyFootDr today!



