Managing Achilles Tendinopathy
Achilles tendinopathy refers to a painful condition characterised by tissue damage and pain in the Achilles region (posterior aspect of the heel and ankle). The muscle group at the back of the lower leg is commonly called the calf.
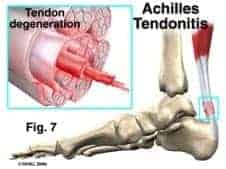
The calf comprises of 2 major muscles one of which one originates from above the knee joint (gastrocnemius) and the other of which originates from below the knee joint (soleus). Both of these muscles insert into the heel bone via the Achilles tendon (see figure below).

Causes for Achilles Tendinopathy
During contraction of the calf, tension is placed through the Achilles tendon. When this tension is excessive, due to too much repetition or high force, damage to the tendon can occur. This damage to the tendon subsequently causes degeneration and inflammation. This may occur traumatically, due to a high force going through the tendon beyond what it can withstand, or due to gradual wear and tear associated with overuse.
Symptoms Of An Inflammed Achilles Tendon
This condition may present as pain and swell at the insertion of the Achilles tendon into the calcaneus (heel bone) or at the mid-portion of the tendon, approx. 5cm from insertion into the calcaneus (heel bone). It can also lead to limited motion throughout the ankle.
There are two classifications of injuries that fall under tendinopathy:
- Tendinitis-an inflammation of the tendon. (This term has previously been used to describe any injury to the tendon and although this term is used often, most cases of tendinopathy are not associated with significant inflammation.)
- Tendinosis-microtears (tiny breaks) in the tendon tissue with no significant inflammation.

How can we help with Achilles Tendinopathy
Achilles tendinopathy is most commonly brought about through physical activity or a sudden change in activity such as increasing the distance of a daily run. This condition causes degeneration of the tissue and means that the Achilles tendon does not possess its normal tensile strength and may be liable to rupture with continued sporting activity.
It is important to fully assess the biomechanical function of the lower limbs in managing this condition. An in-depth analysis is required to assess foot motion with respect to the lower limb, along with assessing the range of motion to determine any muscle tightness. The biomechanical observations can give clues to whether any of the muscles are being overworked or fatigued.
Care Management may include:
- Appropriate stretches
- Strengthening exercises
- Home Care Treatments
- Strapping
- Footwear changes and modifications
- Wear custom made foot orthotics prescribed by a podiatrist
- Commit to a regular checkup from your podiatrist
- Shockwave
How can we help?

Shockwave Therapy
At My Foot Dr Singapore, we use shockwave therapy to manage Achilles tendonopathy, plantar fasciitis/fasciopathy, painful trigger points, and other musculoskeletal disorders of the foot and lower limb.

Custom Foot Orthotics
Our custom foot orthotics are manufactured with precision from digital foot scans and are typically available on the same day.

Video Gait Analysis
We use this advanced form of motion analysis to assist us in diagnosing complex motion-related pathology of the foot, ankle, knee, hip, and lower back.
