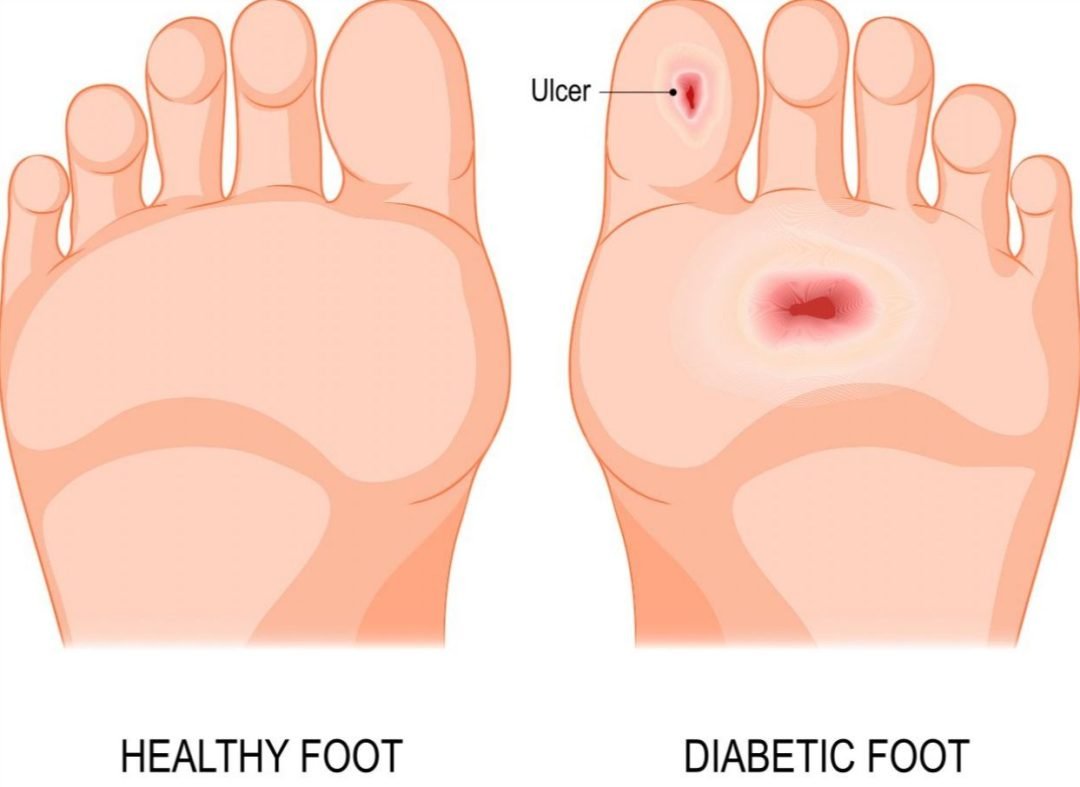
Diabetic foot ulcers are open sores or wounds that are usually located at the bottom of the foot and affect approximately 15 percent of diabetic patients. Diabetic foot ulcers are not often seen as a threat, their symptoms are usually dismissed as trivial. However, these symptoms can have severe consequences if ignored and left unmanageed.
- Infected ulcers can result in amputation if neglected.
- The cost and healing time increase when an ulcer is left unmanageed and deteriorates; it would cost patients $2000 – $3000 to manage an infected ulcer and up to $45,000 for amputation should the situation worsens.
But, good news is that, with prompt care management, up to 80% of diagnosed cases can recover.
Early diagnosis and efficient care management of diabetic foot ulceration is essential in order to avoid limb amputation and to preserve the quality of life for diabetic patients.
What Causes This Condition?
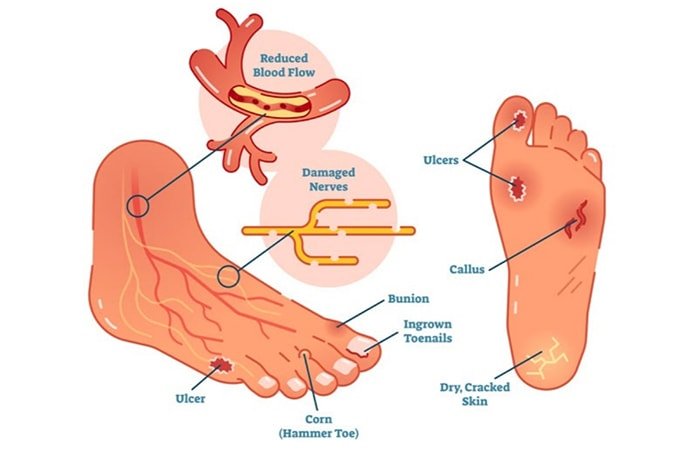
The first cause of foot complications in a diabetic patient is nerve damage from diabetes, causing numbness, and a lack of feeling in the foot and leg. Also known as peripheral neuropathy, it is caused by chronically high blood sugar which damages nerves, reducing their ability to carry signals between the brain and other parts of the body.
Peripheral artery disease is another major condition that happens in diabetics and affects the blood vessels supplying the skin, or medically known as microangiopathy. Diabetic patients tend to have narrower arteries, which affects blood supply to the feet. Thus, a lack of healthy blood flow may cause ulceration and impaired wound healing.
How does a Podiatrist Help with Diabetic Foot Ulcers?
Your podiatrist will ask about your symptoms and examine your feet, footwear and the ulcer. The goal of care management is to start healing your foot ulcer as soon as possible. The risk for infection decreases with faster healing.
- Debridement
- Pressure offloading
- Infection prevention
Ulcer debridement is conducted to remove unhealthy tissue from the wound. This will spark the body’s natural healing mechanism.After the removal, a wound specific dressing will be applied to protect the wound while it heals and promote an optimal healing environment
One essential part of the care management process is to utilise pressure-relieving orthotic devices combined with diabetic friendly footwear.Some individuals may require custom footwear, TAG braces, soft or total contact casts, to offload pressure from the wound in more severe cases.
Failure to reduce load and pressure will result in the ulcer deteriorating and impede the healing process.
What to Watch Out For?
If you have diabetes, poor circulation or peripheral neuropathy, examine your feet every day. Call your podiatrist promptly if you see an area of:
Corns and Calluses
Diabetic foot ulcers are commonly caused by repetitive stress over an area that is subject to high vertical or shear stress. If a corn or callus presses into the foot, it destroys inner layers of skin and fat. Blisters, cracks and sores may form. These open wounds become ulcers. They provide a way for infections to enter the body.
Stained Sock? Beware!
Stains on socks is a warning sign of bleeding or wound drainage. A patient’s foot should be examined and manageed as soon as possible.
Redness or Swelling
If you notice unusual swelling or redness, this is a clear indication that there is something wrong and you have injured your foot unknowingly.
Numbness – loss of sensation
- Common symptom of nerve damage or diabetic neuropathy.
- Caused by poor blood sugar control
Tingling – heightened sensitivity to touch
- Also caused by diabetic neuropathy
- It could also transition from minor prickles to deep stabs of pain.
Muscle weakness
- The lack of blood supply to the nerves affects the way your muscles move, leading to a lack of energy in your limbs.
- According to a study, neuropathy usually affects the muscle strength of the ankle dorsi-flexors and plantar-flexors; you might experience difficulties in walking or standing.
Here are ways to control the occurrence of the aforementioned symptoms and developing ulcers:
- Make it a habit to inspect your feet and socks every day. That will help you spot problems early before they get worse. Use a mirror if you have difficulty bending down to check on your feet.
- Receive prompt care management of foot conditions such as dermatitis, cracked heels, blisters or corns.
- Wear comfortable and properly fitted shoes and socks to protect and improve air circulation around the feet.
- Control your blood sugar and adhere to prescribed nutrition plans, which will reduce diabetic symptoms
- Reduce and eventually cease smoking habits to minimise smoking-induced oxidative stress, which may lead to ulcer development.
Seek Care Management In The Early Stages
There are multiple factors that can lead to diabetic foot ulcers; if you are unsure what your risk status is in developing diabetic ulcers, book an appointment with My FootDr Singapore for a diabetic foot assessment.
The Podiatry team at my FootDr Singapore are all highly trained and skilled at managing diabetic foot ulcers and will guide you through preventive strategies.